ORIF Proximal Phalangeal Fractures
Fractures of the proximal phalanx are potentially the most disabling fractures in the hand. Direct blows tend to cause transverse or comminuted fracture, where as twisting injury may cause oblique or spiral fractures. Proximal phalanx fractures typically present with volar apical angulation because of the the extrinsic and intrinsic muscle tension. Typically the proximal fragments are flexed by the bony insertion of the interossei into the base of the proximal phalanx while distal fragments tends to be pulled into hyperextension by the central slip acting on the base of the middle phalanx.
Most frequent complication of this type of fracture is extensor mechanism adhesions with subsequent loss of motion. The periosteum of the proximal and middle phalanges form the dorsal wall of fibro-osseous tunnel in which flexor tendon glide, when violated by a fracture flexor tendon adhesions may develop and reduce motion in this manor as well.
Case #1 Transverse Fracture Proximal Phalanx Little Finger
 Transverse fracture of the left little finger proximal phalanx with extreme displacement dorsally of the distal fragment.
Transverse fracture of the left little finger proximal phalanx with extreme displacement dorsally of the distal fragment.
 Lateral view showing the sever degree of volar apical angulation.
Lateral view showing the sever degree of volar apical angulation.
 Severe crushing injury which resulted in open wounds as well as the phalangeal fracture, fortunately there was no direct extensor tendon injury.
Severe crushing injury which resulted in open wounds as well as the phalangeal fracture, fortunately there was no direct extensor tendon injury.
 Closed wounds. Eschar on the dorsal hand was allowed to heal by secondary intention.
Closed wounds. Eschar on the dorsal hand was allowed to heal by secondary intention.
 Plate and screws placed dorsally to fixate the fracture.
Plate and screws placed dorsally to fixate the fracture.
 Oblique x-ray showing 4 hole plate and screws traversing the fracture site.
Oblique x-ray showing 4 hole plate and screws traversing the fracture site.
 Full extension postoperatively.
Full extension postoperatively.
 Flexion returning. Patient still receiving hand therapy as evidenced by the hooks glued to his nails on the ring and little finger used for dynamic flexion.
Flexion returning. Patient still receiving hand therapy as evidenced by the hooks glued to his nails on the ring and little finger used for dynamic flexion.
 Lateral post-oerative view of hand making a fist.
Lateral post-oerative view of hand making a fist.
Case #2 Spiral Oblique Fracture Little Finger
Spiral oblique fractures lend themselves to repair with a lag screw technique which involves typically placing two screws across the fracture site. One perpendicular to the fracture site and the second perpendicular to the long axis of the bone. The technique also involved over-drilling one cortex of the bone so the screw threads only capture the distal cortex on the other side of the fracture thereby compressing the fragments when tightened. This type of reduction generally leads towards primary bone healing instead of secondary.
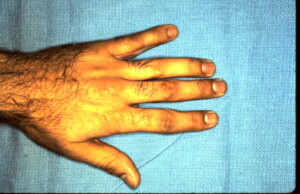 Deviation of the little finger away from the ring finger indicates that the fracture is either angulated or rotated.
Deviation of the little finger away from the ring finger indicates that the fracture is either angulated or rotated.
 Same abnormal posture of the little finger palmar view.
Same abnormal posture of the little finger palmar view.
 Spiral oblique fracture seen on x-ray confirms suspicion raised by grossly abnormal posture of the little finger and tenderness.
Spiral oblique fracture seen on x-ray confirms suspicion raised by grossly abnormal posture of the little finger and tenderness.
 Intra-operative view of reduced fracture held in position with a bone clamp in preparation of placing lag screws.
Intra-operative view of reduced fracture held in position with a bone clamp in preparation of placing lag screws.
 Lag screws in place maintaining anatomic reduction.
Lag screws in place maintaining anatomic reduction.
 Tenodesis effect is checked intra-operatively to confirm that the rotatory deformity has been corrected. The wrist is flexed which causes extension of the digits.
Tenodesis effect is checked intra-operatively to confirm that the rotatory deformity has been corrected. The wrist is flexed which causes extension of the digits.
 The wrist is then extended which causes flexion of the digits. Normal positioning of the digits is noted. the angulatory deformity secondary to rotation has been corrected.
The wrist is then extended which causes flexion of the digits. Normal positioning of the digits is noted. the angulatory deformity secondary to rotation has been corrected.
Case #3 Proximal Phalanx Fracture Ring Finger
 Pre-operative view showing deviation of an injured finger secondary to a spiral oblique fracture of the proximal phalanx.
Pre-operative view showing deviation of an injured finger secondary to a spiral oblique fracture of the proximal phalanx.
 Hyper-extension of the distal fragment is evident secondary to the pull of the extensor mechanism on the distal fragment and the intrinsics on the proximal fragment causing volar apical angulation as well.
Hyper-extension of the distal fragment is evident secondary to the pull of the extensor mechanism on the distal fragment and the intrinsics on the proximal fragment causing volar apical angulation as well.
 Spiral oblique fracture proximal phalanx ring finger.
Spiral oblique fracture proximal phalanx ring finger.





